Aneila Vargas
Clermont, Florida (United States)
ANEILA VARGAS
Scleroderma Stories Issue 5

Please introduce yourself
My name is Aneila Vargas Pagán. I am 28 years old. I was born in Puerto Rico, but I moved to Florida almost 6 years ago. In May, I graduated with a bachelor’s degree in Health Services Administration. I also love to draw!

Could you please tell us about your journey toward being diagnosed?
The first symptom I noticed was two instances of skin discoloration — one on my hand and one on my body. I noticed the skin on my fingers would break, peel, and bleed. Because I worked as a barista at the time, I thought it was because of the exposure to chemicals or because of the hot and cold temperature difference. Not thinking much of it, I just started applying creams at night and wearing gloves.
Then, I noticed I was sleepier than usual and that I was developing patches on my face that resembled rough crocodile skin. At this point, my family told me to see a doctor, but their diagnosis was that these problems were stemming from me being overweight. I ended up visiting three primary care centers. After some tests on my liver, the third doctor diagnosed me with fatty liver disease.
The diagnosis didn’t solve any of the problems I was feeling, and at this point, my hands also became extremely bony, so I finally visited a rheumatologist. She sent me for a test in California that checks for 60 different types of autoimmune diseases, which is finally when I got my scleroderma diagnosis. This July, it will have been three years.
Alongside scleroderma, my doctors diagnosed me with polymyositis, which, broadly, is irritation and inflammation of the muscles. This explained a lot of the pain and fatigue I was feeling. It also was causing the fatty liver misdiagnosis; my muscles and sinuses were inflamed, not my liver!
What treatments and medications have you tried? What has worked for you?
I am currently on Cellcept. It is normally prescribed to patients who undergo organ transplants, which is why I was initially nervous to start taking it. It lowers the patient’s immune system, which was tough for me since I got COVID-19 four times during the height of the pandemic.
I take oral steroids for my polymyositis. It controls cortisol levels and slows down muscle inflammation, but its side effects include weight gain, especially around the face, creating the term “Moon Face.”
I also take Plaquenil to regulate the pain and inflammation in my hands, which is caused by arthritis. Finally, I was diagnosed with Raynaud’s syndrome, but living in Florida has kept it under control. I was prescribed Amlodipine, which is a medication for heart conditions, since it deals primarily with blood flow, but I have not had to take it.
Sometimes, changes in my diet or environment can cause a flare-up in my symptoms, so my doctor will raise or lower my doses accordingly. Overall, my treatment plan has definitely improved my symptoms. The medication for polymyositis, especially, is really effective. Sometimes, there are days when I forget about the pain.
What lifestyle changes have you made?
Being from Puerto Rico, I used to practically live on the beach. The high sun exposure, however, means I can no longer go because CellCept heightens my risk of skin cancer. I don’t think I’ve gone in almost two years. I have also modified my diet. I steer clear of gluten, since it seems to aggravate my symptoms. Being in large public spaces is also difficult because I am much more exposed and prone to get ill from someone who may just have a small cough.
I have also started to lift weights — nothing crazy— to keep my muscles active, especially because of my polymyositis diagnosis. Basic things like opening bottles, as well as larger things like contributing in the house, have become harder. I often have to communicate to my partner that I am low on energy, which is why I struggle with these things.
How did you manage your mental health and emotions following your diagnosis?
During the first year, I was very emotional. I was especially angry at myself, and I would deprive myself of joy. I felt like I didn’t deserve to enjoy life anymore or that by making time for others, I would only hurt them more in the long term if I passed away. Over time, I have had to learn how to enjoy life and simply be more caring towards myself.
My drawings posted on my Instagram page also represent exactly how I am feeling at that moment. It’s like satire. I’m making fun of myself, which becomes an outlet for my feelings. For example, one drawing was a before and after of using one of the oral steroid medications that made me gain a lot of weight, while other drawings are more fun or encouraging, which reflects a time when I felt great about myself.
What changes to your mindset has your diagnosis brought about?
My initial diagnosis was actually quite defeating. I struggled to find support groups. There was information, such as on WebMD pages, but no one to connect with, which made me feel worse. I felt a sense of desperation to meet someone else that would understand being diagnosed with something that most people have never even heard about.
This prompted me to create the Instagram page called @agirlwithscleroderma. I already love to draw and hadn’t been able to for a long time, so the initiative pushed me to find a creative outlet. After posting my first few drawings, random people would stumble across the page, giving me organic chances to connect with them.
The first year was mostly a grieving process. I thought a lot about things I could do in the past that are inconceivable now or about the side effects of my medications, which limited my perspective significantly. Ultimately, I leaned into my family and my partner to get an extra push. After speaking with other scleroderma patients, however, I feel really lucky that I feel relatively good on a daily basis. So many people that I have met cannot properly manage their symptoms or were diagnosed years after the onset of their symptoms. Being grateful for where I am has helped me keep my positive mindset.
How have you connected with the online scleroderma community?
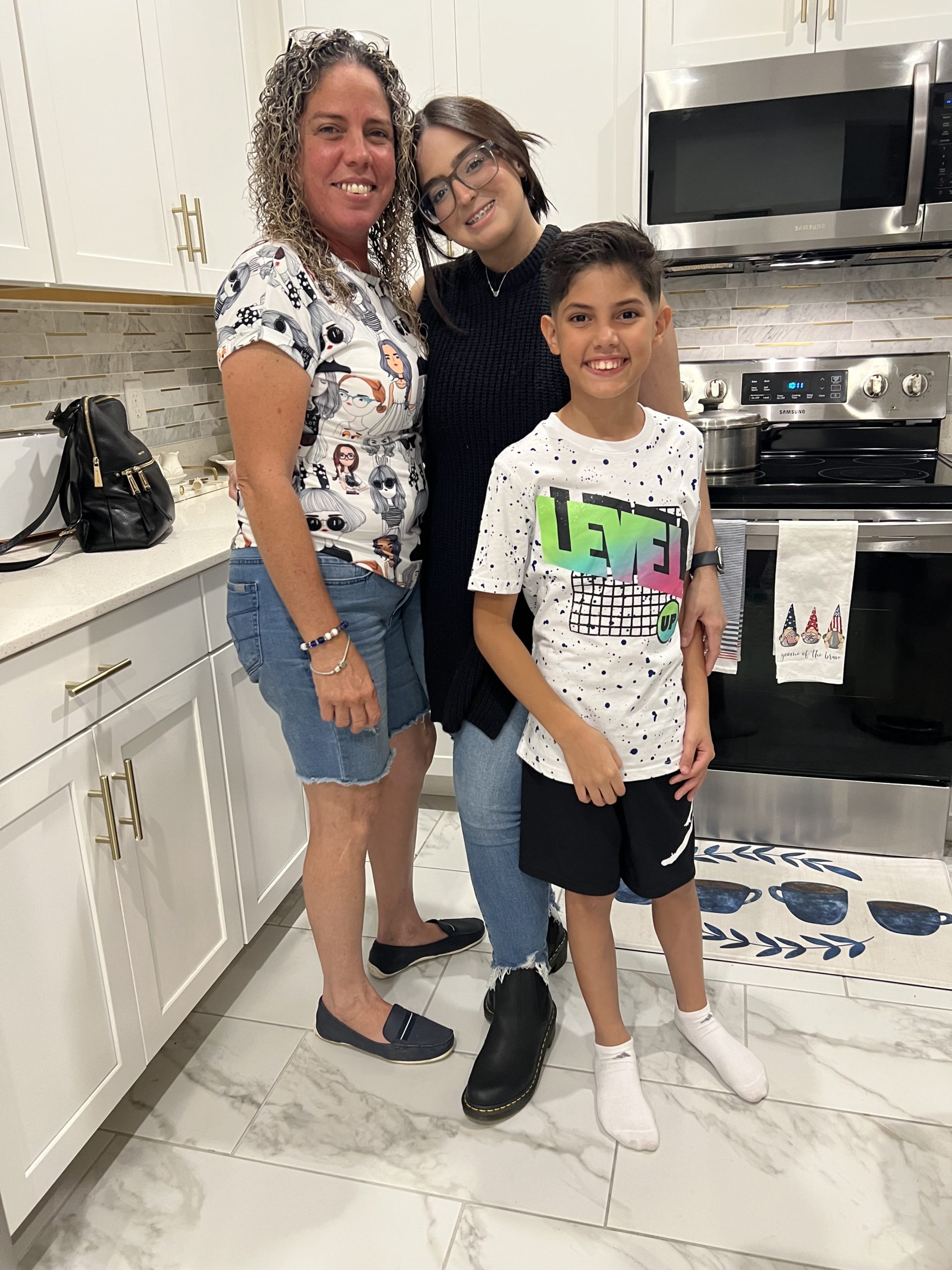
A woman named Lauren from the Scleroderma Foundation reached out to me after seeing my art on the Instagram page. Speaking to her was my first real chance to share my story. She connected me to the Foundation’s therapists and counselors; different Facebook groups, such as for caregivers or for diagnosed patients; and the Foundation’s Florida chapter, which held Zoom meetings every once in a while.
Tell us more about your Instagram page, @agirlwithscleroderma!
When I first created the page, I never intended to show my face. You’ll see there aren’t any pictures of me posted. I think I was coming from a place of shame. I didn’t look like many other scleroderma patients. I figured I would never have to show my face if my drawings could convey how I was feeling. Now, I am leaning towards showing my face on the page because I am more aware of the fact that the aggressive nature of the disease means it affects every patient differently.
Then, people who were not diagnosed but were experiencing key symptoms started contacting me. It was quite overwhelming. They would ask, “Who did you see? What medications are you on? Which ones should I take?” This desperation that others felt was exactly what I initially felt. For them, finding someone experiencing what they were going through was a foot in the door towards diagnosis.
I have a lot of Spanish-speaking followers, which I take great pride in. The content is quite limited for this community, so I can play a small role by translating information for patients and families.

What are your hobbies and interests? How did your diagnosis affect your level of engagement with these?
I love reading, watching a whole variety of shows, all kinds of drawing and related art, and growing plants. I’m a total homebody! When it comes to art, I’ll do more than just drawings. I can edit pictures, create clay sculptures or objects, and a lot more!
Because scleroderma affected my hands, I thought that with the resulting arthritis, I wouldn’t be able to use my hands in the same way as before. Luckily for me, however, the medication kicked in early in my treatment plan, which means my hands have been in pretty good shape so far. Some days, there is more general pain, but I can compensate for that by taking a break from the art for some time until I feel strong enough to continue.

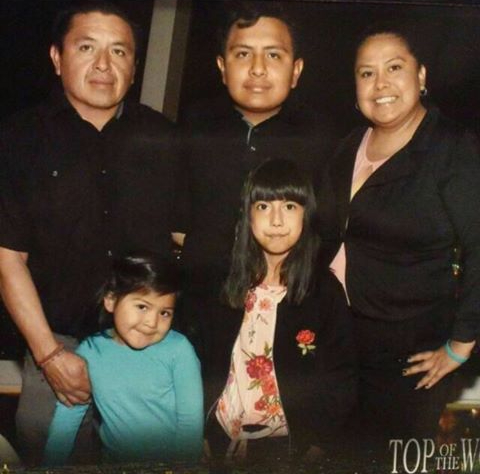
How has your diagnosis affected your relationships with loved ones?
My cousin was the first person who told me to go see a doctor after I started showing symptoms, but my entire family has been incredibly supportive, despite most of them living in Puerto Rico. When I had to get my surgery, for example, and I mentioned it in the family group chat, everyone said “WE’RE getting the surgery.” That level of support is unreal.
I am also engaged to my partner of five years, who I met at the law firm we both work at. He has definitely been a rock for me. I feel like something that is really important but isn’t often talked about is how a diagnosis can affect your partner. He basically went through similar stages of grief that I did. It’s very challenging for them to understand that their partner may not always look and feel their healthiest. He has always picked me up when I cannot do the things I normally love to.
I didn’t realize this before, but my diagnosis affects my ability to get pregnant. I am currently considered high-risk. I am able to conceive, but I would need to be off medications for 3 months before trying, and then the entire pregnancy as well as breastfeeding journey. It would put a huge weight on my health.

What about your ability to continue with school/work?
I work from home, which has been one of the biggest advantages throughout my journey following my diagnosis. If I don’t feel good one morning, I can work from the bed, be there all day to rest, and still get all my work done.
Being busy with school helped distract me from how I felt about my diagnosis. At the time, I was going through my summer semester, and I didn’t stop to process or acknowledge my feelings. In the moment, I was able to grieve that way, although in hindsight that may not have been the best.
Often, I was really exhausted. I had work, online classes, and homework, along with helping around the house and spending time with my partner. It felt like everyone else had a 24-hour day, while mine was much shorter. I would get tired much quicker.
What advice do you have for other scleroderma patients?
Often, patients don’t have proper information regarding providers or centers they can go to for help. They assume they have to go to places approved by the National Scleroderma Foundation. My current doctor, however, is not listed under that designation, and my care plan is truly the best it can be for me.
People who are on waiting lists for appointments at the Mayo Clinic or for months out from the status quo cannot afford to take the risk of waiting that long. I try to direct patients to regular rheumatologists while they maintain their positions on these waitlists so they are still at least being regularly seen in the meantime. Another hack for me has been Cost Plus Drugs, which Mark Cuban from Shark Tank created! It has helped me afford the medications I am currently on. All I need is a prescription, and appropriate refills are taken care of.

Be sure to follow us on Instagram and Facebook (@sclerounited) to see more scleroderma warriors’ journeys in our weekly Sclero Sunday series.
Are you a scleroderma warrior? We’d love to interview you for Scleroderma Stories! Please visit tinyurl.com/share-my-sclero-story or email us at contact@sclerounited.us